The other day, I was on the internet, loosely surfing about precision medicine. I found an article in Critical Care Medicine in which several cool authors from cool North American universities outline methodological approaches for assessing treatment effect heterogeneity.
Did I write cool? Mmm… I am pretty confident none of them surfs. Moreover, they are not Brazilians. It's common sense we are the coolest people on Earth. What? Canadian? Sorry. You are not cool, ok? It sucks to walk through tunnels home to work and back home instead of commuting on the surface.
Anyway. Let’s move to today’s episode.
The latent rationale is that treatment effects are expressed as means, so the information on individual responses is lost.
Therefore, according to the rationale, we should identify the responders and prospectively test the intervention only on the responders. To make it cooler, call the different responders “phenotypes” or other words finished with “-types”.
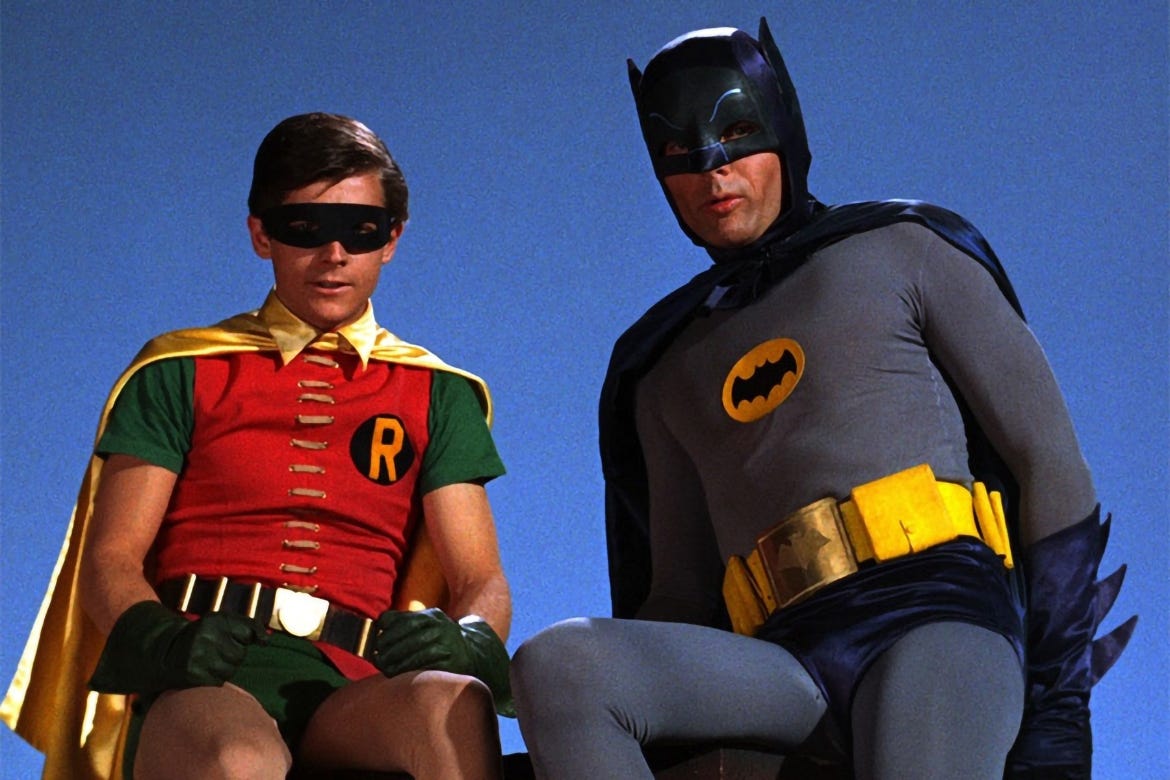
Holy innocence, Batman!
“You know, Robin, my utility belt is seemingly infinitely stocked with cool gear.”
“I knew it Batman”
“In this episode, we will reopen dead files from critical care studies and look at the data through my precision lens”
“Incredible idea, Batman. What for?”
“We will find new patterns in the data”
“Wow! You’re so smart, Batman”
“I know”
The 17th episode of The Thoughtful Intensivist has begun! Are you ready? Go!
Let's talk about Anakinra. No, kids. Listen. Anakinra is no Batman’s arch-rival. It’s a drug. I know it’s the coolest name for a drug but it’s time to get serious.
Anakinra inhibits IL-1B receptors. In macrophages, it effectively reduces the switch to the pro-inflammatory phenotype M1.
Anakinra was tested in sepsis during the cytokines hype of the 1990s. By that time, researchers resolved to test the then-young sepsis definitions. It was time to test anti-inflammatory agents.
They had recently tested methylprednisolone for sepsis and it didn’t work. In this context, interest turned to cytokines. Studies reported serum cytokines levels, and phrases like “cytokine storm” circulated among well-read intensivists. In 1997, an RCT by Dr. Opal's research group tested anakinra to block the effects of IL-1B in septic patients. It failed to show a benefit.
A reappraisal of the clinical trial emerged in 2016. This time, the authors were smarter. They knew there was a sepsis subgroup with features of macrophage activation syndrome (MAS). Their hypothesis was plain and highly plausible: anakinra reduces mortality in septic patients presenting MAS. They showed it does.
This is the best reanalysis I have ever seen. The first author Dr. Bita Shakoory has my perpetual applause. What a f* good work!!
They established subgroups based on actual phenotypes. It’s safe to say they told MAS patients from the other infected patients. More than a sepsis mimic or sepsis phenotype, MAS is an actual disease with a sound disease model. Sepsis is not.
So far, so good. Let's compare it with the Crystal-ball subgroups popping up in critical care journals.
I recently devoted a post to the PRECISE Study. The authors took a dataset and performed a post-hoc analysis to search for any positive association between a few invented sets of vital signs and the response to an intervention, namely giving a balanced solution instead of saline. Of course, they found an association. You always find an association if you test enough variables or variable combinations.
It is obviously a spurious crystal-ball association because it was not based on real-life biology like the MAS study. It could have been the horoscope, preferred rock band, preferred Marvel hero, or the number of minutes waiting for the Uber driver in the last week.
Unfortunately, they are testing the subgroup they pompously named "Group D phenotype" on a prospective saline vs balanced solution RCT.
"Squared bullshit, Batman!"
A Crystal-ball subgroup analysis is a post-hoc subgroup analysis that doesn't care about human biology. Researchers just run the analysis to see what happens.
Did you think P-fishing?
I found a more nuanced and complicated attempt to establish "precision medicine” subgroups in ARDS patients. The paper was recently published in the Chest Journal.
Many of the authors are cool people per nationality criteria. I split them into two Coolness Phenotypes using the nationality criteria, The Brazilians and The Rest. We could prospectively test if they perform differently on a sunny beach. What a strong hypothesis! Do you agree? Hint: this one doesn't need to be biologically plausible.
Back to the paper. An earlier study had "discovered" two ARDS phenotypes and named them subphenotypes A and B. The previous study used nine variables to identify the subphenotypes (pH, PaO2, creatinine. bilirubin, bicarbonate, MAP, HR, RR, FiO2). Subphenotype B had higher IL-6 levels and hence was called hyperinflammatory.
In the Chest study, the authors reanalyzed data from two ARDS RCTs reclassifying the patients into phenotypes A and B. They found that phenotype B benefited more from higher PEEP than phenotype A.
How can bilirubin, creatinine, HR, MAP, etc relate to PEEP response? Please draw.
"Does this sphinx have a secret?" I wonder, recalling Oscar Wilde's metaphor.
This is a quite elegant study. Its methods have all the complicated analysis you can dream of. Half-Baked Hypotheses demand lengthy and complex Methods sections, like the explanations you read in a text beside an ugly painting in a museum.
The Discussion section, however, is fun. There, and sometimes in the accompanying editorial, are the despairing Backward Reasoning exercises. The nature of the study appears in its naked entirety. The authors don't know how to justify the biological plausibility of the data they just presented.
I discussed three instances of post-hoc phenotyping. The studies included only patients fulfilling the invented threshold definitions for sepsis or ARDS. All patients have in common being first lumped as sepsis or ARDS irrespective of “phenotypes” and then split into subgroups.
For instance, the original anakinra study misses all MAS patients who did not fulfill the guessed sepsis thresholds. Likewise, the original ARDS studies excluded all hypoxemic respiratory failure patients who did not meet the arbitrary ARDS thresholds and included all who met them, regardless of the "phenotype". Selection bias contaminates the studies and prevents us from finding useful disease models for sepsis and ARDS.
This is the Petty and Bone mistake. It will sink the precision critical care enterprise, in the same way it trashed decades of research on ARDS and sepsis. No crystal ball is needed to foresee the failure.
We see the precision medicine wave rising from a distance. Our surf skills will shape the next decade. Did you ever surf? It is the coolest thing on Earth.
We risk missing the precision medicine wave because we intensivists are terrible bad surfers.
“I see you are riding the precision medicine wave, Batman!”
“Learn from me, Robin!”
Thank you for reading The Thoughtful Intensivist!








Petty and Bone taught all of us to surf. Who knew they didn’t know how to ride the waves.
I’ve surfed several waves over the years in critical care. I understand, and support, what you explain so well, because I have “suffered” it. I couldn’t agree more.